Living With Polio
Definitions
Technically, post-polio syndrome is not the same condition as Post-Polio Sequelae/ the late effects of polio. Post-polio syndrome is usually considered a specific new condition. A diagnosis of exclusion is used to determine if a patient has PPS. This means if a survivor of polio is found to have osteoarthritis, for example, that is what the diagnosis will be – osteoarthritis, not PPS. Because of this, the number will be lower for post-polio syndrome than when the number is referring to post-polio sequelae or the late effects of polio.
Twenty-five to forty percent of polio survivors experience post-polio syndrome (depending on the study).
As many as 70% of polio survivors are said to have Post-Polio Sequelae or late effects of polio.
Don’t Get Hung up on Definition
Polio conditions exist along with other diseases. Therefore, it is important not to get hung up on definition but to encourage polio survivors and their medical professionals to work together to find the causes of any symptom and provide treatment, i.e., medication for hypothyroidism, hypertension, diabetes, irritable bowel syndrome, etc., etc. An evaluation that too quickly determines that prior polio is the sole cause deprives survivors of potential treatments.
Post-Polio Syndrome
Post-polio syndrome is a new condition that affects the survivors of polio decades after the acute illness of poliomyelitis. The major symptoms are pain, fatigue and weakness. New weakness is considered the hallmark of post-polio syndrome. Less commonly, survivors may have new sleep/breathing/swallowing problems and some survivors may also experience muscle atrophy or muscle wasting.
Criteria for Diagnosis
The criteria for diagnosing post-polio syndrome have evolved over the last 20 years. The United States National Institute of Neurological Disorders and Stroke (NINDS) lists the following Criteria for diagnosis of post-polio syndrome*
- Prior paralytic poliomyelitis with evidence of motor neuron loss, as confirmed by history of the acute paralytic illness, signs of residual weakness and atrophy of muscles on neuromuscular examination, and signs of nerve damage on electromyography (EMG). Rarely, persons have subclinical paralytic polio, described as a loss of motor neurons during acute polio but with no obvious deficit. That prior polio now needs to be confirmed with an EMG. Also, a reported history of nonparalytic polio may be inaccurate.
- A period of partial or complete functional recovery after acute paralytic poliomyelitis, followed by an interval (usually 15 years or more) of stable neuromuscular function.
- Gradual onset of progressive and persistent new muscle weakness or abnormal muscle fatigability (decreased endurance), with or without generalized fatigue, muscle atrophy, or muscle and joint pain. Onset may at times follow trauma, surgery, or a period of inactivity, and can appear to be sudden. Less commonly, symptoms attributed to PPS include new problems with breathing or swallowing.
- Symptoms that persist for at least a year.
- Exclusion of other neuromuscular, medical, and orthopedic problems as causes of symptoms.
*Modified from: Post-Polio Syndrome: Identifying Best Practices in Diagnosis & Care. March of Dimes, 2001.
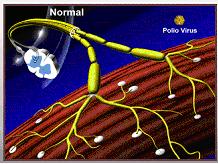
WHAT CAUSES POST-POLIO SYNDROME? In the early years, there was some speculation that the cause might be a “recurrence” of polio or reactivation of the poliovirus, which is not the case. The generally accepted theory is best demonstrated by the following diagrams.**
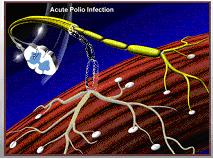
1. Degeneration of Nerve cells (Neurons) during Acute Polio
|
Diagram of healthy spinal cord section with nerve cells (motor nerve cells) branching to muscles.
|
 |
|
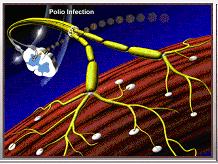
During acute polio infection the nerve cell is invaded by poliovirus.
|
 |
|
In this diagram, one of the nerve cells has been infected by the poliovirus, while its neighbor has not.
|
 |
|
Destruction of the infected nerve cells results a lack of nerve supply to the muscles.
|
 |
|
If this process occurs on a large enough scale, it can result in loss of muscular function, and can cause weakness or paralysis.
|
 |
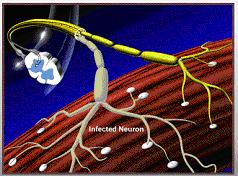
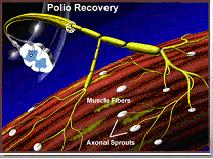
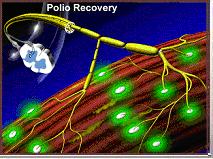
2. Recovery From Acute Paralytic Polio
| Immediately following paralytic polio, surviving motor nerve cells in the brain stem and spinal cord extend new branches to re-connect the nerve cell to the muscle. These are called sprouts. |  |
|
In this diagram, the new sprouts are now capable of triggering contraction in the muscles and muscle function can be partially or fully regained.
|
 |
|
Thus, many motor nerve cells end up supplying several times the number of muscle fibers they would normally supply.
|
 |
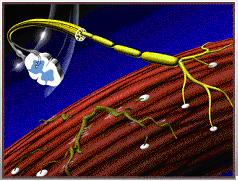
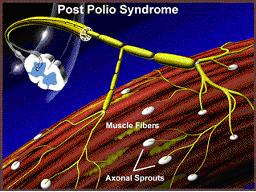
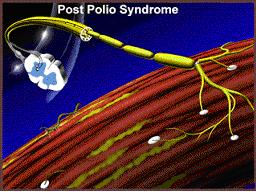
3. Mechanism of Post-Polio Syndrome
|
Wiechers and Hubbell proposed that these new sprouts are not indefinitely stable…Wiechers, D. & S.L. Hubbell. 1981. Late changes in the motor unit after acute poliomyelitis. Muscle & Nerve 4: 524-528.
|
 |
|
…but rather degenerate over time due to an “overexertion” phenomenon resulting once again in muscle fibers that no longer contract, which a survivor recognizes as new weakness and loss of function.
|
 |
**Modified from: Post-Polio Syndrome: A New Challenge for the Survivors of Polio©, Post-Polio Health International (1997)
THE LATE EFFECTS OF POLIO: SURVIVORS
There are 12-20 million other individuals who had polio living in the world today.Although some people think “polio does not exist anymore,” even now the poliovirus is causing poliomyelitis in under-vaccinated children. You may live in a country that is still trying to eradicate the poliovirus and where there are barriers to education, employment and healthcare for survivors. Or, you may live where cases of acute polio no longer occur, but where you have to challenge the status quo that excludes people with disabilities from full participation in life. In either case, for you, polio still exists.
There are long-term physical consequences to having had poliomyelitis. New symptoms recognized by the medical community that may relate to prior polio include:
unaccustomed fatigue – either rapid muscle tiring or feeling of total body exhaustion;
- new weakness in muscles, both those originally affected and those seemingly unaffected;
- pain in muscles and/or joints;
- sleeping problems; breathing or swallowing problems; and/or decreased ability to tolerate cold temperatures.
Any combination of the symptoms may affect your ability to conduct customary daily activities such as climbing stairs, walking, lifting, etc.
Recommended Actions:
Obtain a complete general medical evaluation from your primary care physician. Any medical problems found in the evaluation should be treated and monitored.
If your symptoms persist, seek a neuromuscular examination from a specialist in post-polio problems, typically a physical medicine and rehabilitation specialist (physiatrist) or a neurologist. The purpose of this examination is to determine what the problem is and to establish a baseline from which to judge future changes, to evaluate and update your mobility aids and/or your ventilatory equipment, and to develop an individualized management plan.
Do not attempt to diagnose yourself. Post-polio syndrome is a diagnosis of exclusion and it is important to rule out (or treat) conditions with similar symptoms that may be causing distress.
Although research has not yet identified a medication that stops or delays the weakening of muscles, the symptoms can be managed.
Seek medical advice and use recommended mobility aids and ventilatory equipment.
Listen to your body and follow common sense guidelines that include avoiding activities that cause pain and/or fatigue that lasts more than ten minutes.
Pace yourself in your daily activities, routinely stopping to rest for 15 to 30 minutes several times a day.
Consider joining a support group that espouses self-help and encourages group participation and positive action, or consider seeking individual and/or family counseling to assist in making needed lifestyle changes.
Maintaining health is essential for those with a compromised neuromuscular system. Heed general advice about eating well, getting the proper amount of sleep, avoiding unhealthy habits such as smoking and overeating, and exercising appropriately. Many symptoms result from the overuse and misuse of muscles and joints. Carefully consider which muscles to exercise and how often.
Educate yourself and your loved ones about post-polio problems and treatment approaches. Cultivate a team of traditional and, when appropriate, complementary health professionals, collaborating with them as you strive for health and independence.
THE LATE EFFECTS OF POLIO: FAMILIES AND FRIENDS
The experience of having had poliomyelitis (infantile paralysis) is a very personal one. Having the acute illness can result in no hospitalization to isolation and months, even years, of rehabilitation. Memories of polio vary as well. Survivors who had polio as children may have no conscious memory of the illness or subsequent rehabilitation, whereas some survivors vividly remember the pain and paralysis of the acute infection and their medical treatments. The care differs from country to country, from decade to decade, and from rural communities to cities.
Poliomyelitis is caused by any of three serotypes of poliovirus. The major illness types include non-paralytic and paralytic poliomyelitis. The poliovirusdamages motor nerve cells and, consequently, the muscles instructed by those nerves are temporarily or permanently paralyzed. Acute polio does not infect sensory nerves, so sensation is not affected. Paralytic poliomyelitis can be classified as spinal, bulbar or spino-bulbar. Bulbar is the most serious form of polio and involves the part of the brain dealing with the vital functions of respiration and swallowing.
The new problems facing your loved one are not caused primarily by thepoliovirus, but are problems secondary to having polio. Polio survivors experiencing new symptoms have not been re-infected nor are they contagious. They need your understanding and support.
Post-Polio Health International recommends that all polio survivors have yearly medical examinations and that those who are experiencing any of the persistent new symptoms of weakness, pain, fatigue and breathing problems obtain a comprehensive neuromuscular examination. Some survivors are reluctant to seek medical attention. Reasons for avoiding a physician can include early memories of polio, a recent visit that was not helpful, belief that no physician today understands the late effects of polio, or an inaccessible office or examination table.
Your role as a family member may be to encourage an evaluation and to assist in implementing the treatment plan.
Polio survivors do not experience new problems in isolation. What affects them can affect you. You will be addressing, possibly for the first time, many issues:
- selecting specialized health professionals and new equipment;
- learning about access and disability laws;
- making choices in how to spend time, energy, and financial resources.
Additionally, long-standing roles may by necessity be challenged or changed.
Understanding and accepting all of the ramifications of the late effects of polio is not easy. No one can predict the future, but it is recommended that you and the polio survivor in your life attempt to approach the concerns as a team that includeshealth professionals.
Polio survivors can have feelings of guilt about being “a burden.” Or, they may feel sadness for “the way things were.” You may feel resentful of your new responsibilities. It is recommended that you address these issues as they arise. Everyone has different skills, methods, and preferences in solving problems. Ascertaining and utilizing these skills can be very beneficial to maintaining a healthy relationship. Many relationships have benefited from an association with a support or self-help group or from family counseling.
Educating yourself about the many facets of the late effects of polio is the first step in determining your role in a management plan grounded in the commitment of your loved one to make lifestyle changes.
©Post-Polio Health International
